Subscribe to trusted local news
If you are accessing this story via Facebook but you are a subscriber then you will be unable to access the story. Facebook wants you to stay and read in the app and your login details are not shared with Facebook. If you experience problems with accessing the news but have subscribed, please contact subscriptions@thestrayferret.co.uk. In a time of both misinformation and too much information, quality journalism is more crucial than ever. By subscribing, you can help us get the story right.
- Subscription costs less than £1 a week with an annual plan.
Already a subscriber? Log in here.
14
Sept 2024
Cash injection needed to end doctor's appointment misery, says GP

Anyone who’s ever had to wait in a caller queue at 8.30am to secure a doctor’s appointment, only to be offered one a week next Thursday – and who hasn’t? – will suspect that change of some sort needs to come to GP surgeries.
That’s certainly not a situation that’s alien to people in our area. This week, the Stray Ferret contacted all 17 GP practices in the Harrogate district to ask how long the current wait is for a non-urgent appointment with a GP.
Ten practices responded, and their answers varied widely. The shortest wait was five days, and the longest was 25 days. The average wait was 13 days.
Quite what any change might look like has been unclear for a long time, but this week the Prime Minister gave notice that it will indeed come.
Responding to the publication of the nine-week Darzi Review into the National Health Service, Sir Keir Starmer warned that the NHS must “reform or die” and outlined a 10-year plan involving some big changes.
One of these is a shift to more neighbourhood care, rather than hospital care, and this, he said, would include improving access to GPs and "bringing back the family doctor".
How this will be done has not yet been revealed – the details will come “over the coming months” – but Dr Brian McGregor believes that any plan will have to tackle the decline in numbers of GPs.
Dr McGregor is chair of the Yorkshire Regional Council (YRC) of the British Medical Association, and a director of Harrogate-based YOR Local Medical Committee Ltd (YORLMC), which represents all NHS GP teams across North Yorkshire and parts of West Yorkshire.

Dr Brian McGregor
He told the Stray Ferret:
GPs are seeing more patients than ever. We’re providing patients with more care, but numbers of GPs are actually falling.
In 2019, GPs provided 1 million appointments a day, but now they provide 1.5 million appointments a day – a 50% increase, but with no more doctors to do the work.
That’s one of the reasons why it’s hard to get a GP appointment – we haven’t grown our GP base in line with population growth.
He said the shortfall in doctors was exacerbated by doctors leaving the NHS, which left those still working much more to do, leading to staff ‘burnout’. He said:
Retention is a big problem. Since 2011, we’ve lost 25% of GP practices. We’re overworking GPs, and that’s not safe. We’ve invested nothing in retaining them and we’re burning them out.
When I qualified in 1987, the average age of retirement for GPs was 65. The average age GPs leave the profession now is 38. They either stop practising or they go abroad to Australia, New Zealand or Canada.
The average GP here works for 40 to 50 hours a week, but if they move to Canada, they can work for 30 hours a week for twice the income. We just don’t value our GPs here.
A major problem, he said, was that there just isn’t enough money in the system to take on more doctors. He said:
We’ve actually got the training and education side sorted out. We train about 4,000 a year, but in August this year, 3,000 of the new graduates couldn’t get a job. It’s just crazy that we have unemployed doctors because there’s no money to employ them.
The previous government put in more funding, so we could employ pharmacists, physiotherapists and physician associates, but we were specifically banned from taking on more doctors.
They thought they’d be freeing up GPs, but with population growth and doctors leaving, it didn’t work. It was disastrous.
He added:
We have a very short window of opportunity – maybe three to five years – to reinvest in general practice and rebuild numbers of GPs.
We can’t wait three years for ‘service reviews’ and the like; we need an injection of cash now, so that we can take on more GPs and increase the supply of appointments for patients.
However, Sir Kier Starmer said on Thursday that there would be “no money without reform”, and that the government had to “fix the plumbing before turning on the taps”.
How that reform will be manifested remains to be seen, but Chris Brackley, who chairs the Patient Participation Group (PPG) for the Spa Surgery in Harrogate, thinks the government will have to reform and pump in cash, quite radically.
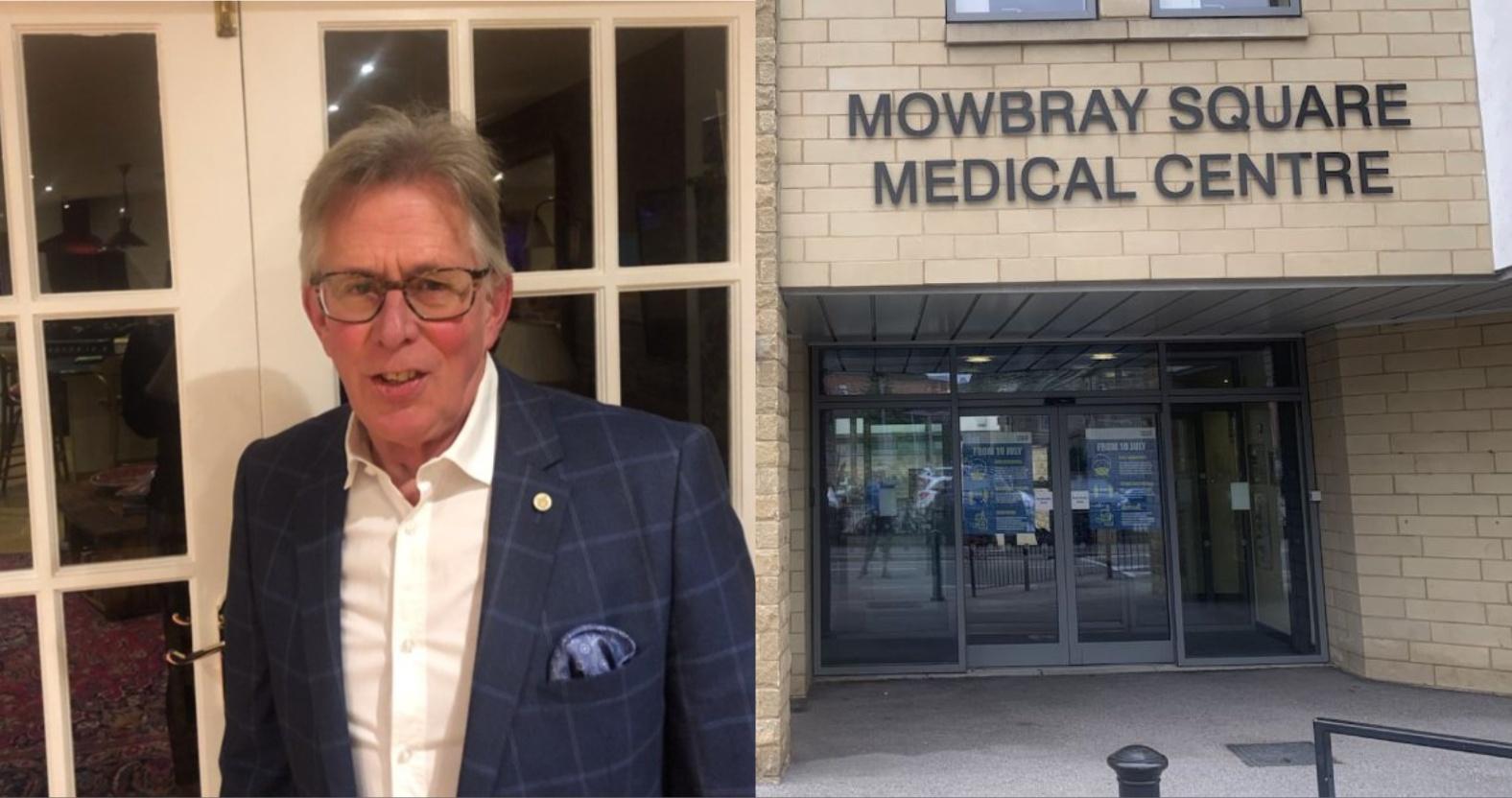
Chris Brackley chairs the Patient Participation Group for Spa Surgery, which is one of three GP practices in the Mowbray Medical Centre in Harrogate.
He said:
The system is in such a mess that some fairly drastic action is needed. I think the government will probably renationalise GP practices and throw a lot more money at the NHS, so they can say ‘look, we’ve cured the GP problem’.
Would that be a problem?
No, it would make sense in many ways. From a patient perspective, it would all be to the good.
Sir Kier also said that the governments’ plans would take at least two terms to enact, and that change would come slowly.
In the meantime, Dr McGregor said that patients could help ease the situation. He said:
I would encourage patients to be kind, always. When people don’t get the appointments they want, they get angry, but GPs want what patients want: to see a GP in a timely manner and in a way that suits them.
Everyone in a GP surgery is working under pressure, especially receptionists, who often earn minimum wage.
Also, write to your MP and encourage them to support investment in GPs, and appreciate that decisions are taken at national level. GP surgeries are doing everything they can behind the scenes to provide patients with what we all want: better access to healthcare.
3